
ELSI

Over ELSI
ELSI is een Engelse afkorting en staat voor Ethical, Economic, Legal and (psycho)Social Issues. ELSI onderzoek binnen de Genetica afdeling van het UMCG is onderdeel van het ELSI programma. Binnen het ELSI programma worden (potentiële) ethische, economische, psychologische, sociale/maatschappelijke en juridische implicaties onderzocht van (nieuwe, veelbelovende) genetische technologie en methodes van diagnostiek, counseling (inclusief eHealth) en screening.
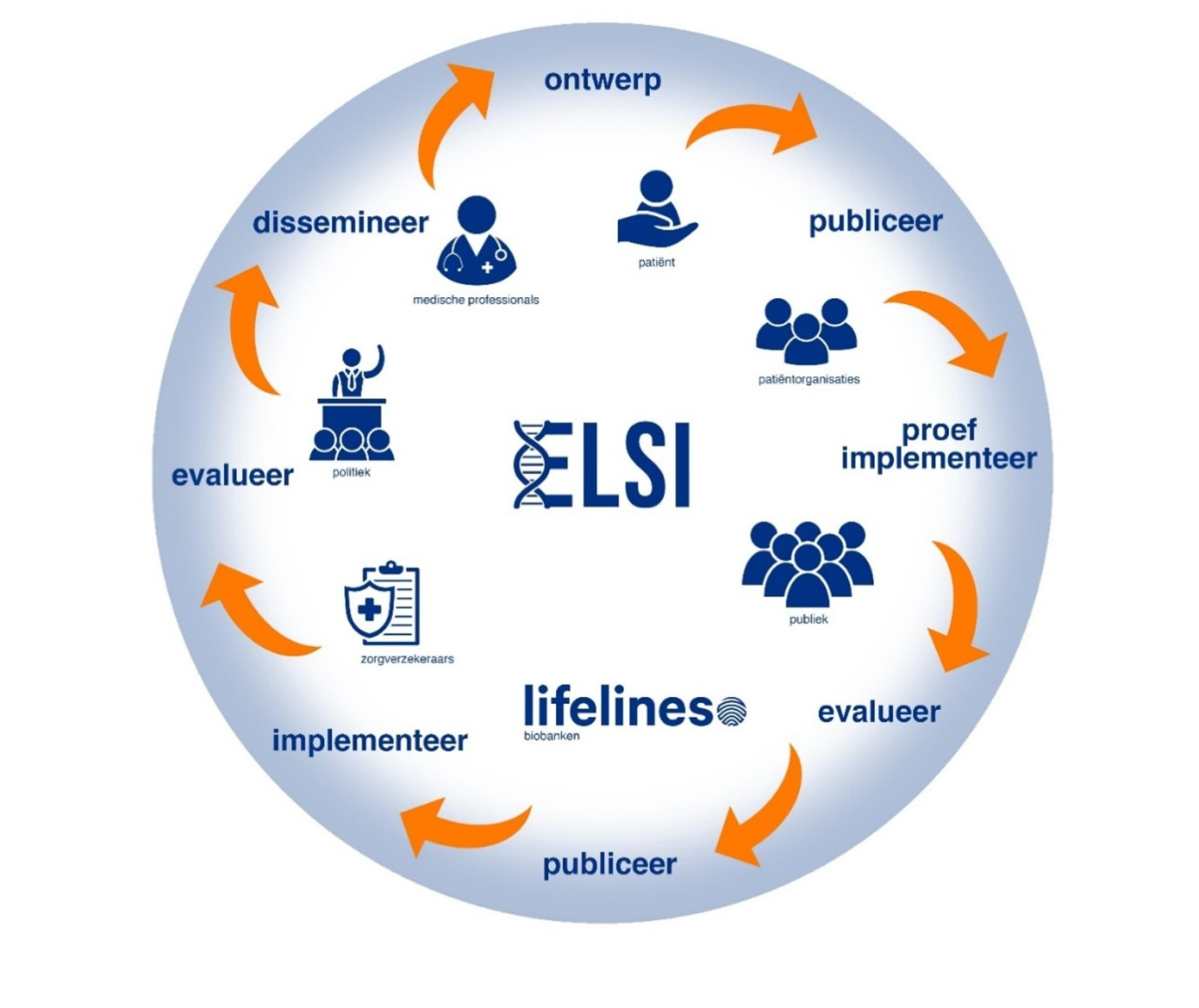
Het doel van het ELSI-programma is om, samen met alle stakeholders, na te gaan of en hoe de eerder genoemde technieken en methoden zo snel en verantwoord mogelijk kunnen worden ontwikkeld en geïmplementeerd in het voordeel van patiënten en het publiek. Het programma is ook bedoeld om hiaten (bv. juridische of financiële) te identificeren die aangepakt moeten worden, voordat verantwoorde implementatie mogelijk is. De ELSI onderzoeksgroep werkt op verschillende thema’s samen met nationale en internationale collega’s. De onderzoeksactiviteiten richten zich op theoretische en conceptuele vraagstukken, maar ook op pilot onderzoeken en vergelijkende trial studies, met als einddoel de translatie van resultaten naar de klinische praktijk (zie ook de figuur met de onderzoekscyclus). Een belangrijk aspect van ons onderzoek is de betrokkenheid van alle belanghebbenden, waaronder ook patiënten en de burger. Meer informatie over deze aspecten kan worden gevonden in de beschrijvingen van onze onderzoeksprojecten. Naast onderzoeksactiviteiten is er binnen het strategisch ELSI-programma aandacht voor moreel beraad, patiëntparticipatie en onderwijs.
Kernteam
Dr. Imke Christiaans PI/programmaleider (klinische genetica, epidemiologie)
Dr. Els Maeckelberghe (ethiek)
Prof. Adelita Ranchor (psychologie)
Dr. Erwin Birnie (economie, epidemiologie)
Dr. Mirjam Plantinga (economics, ethiek, sociologie)
Dr. Jacobien Niebuur (postdoctoraal onderzoeker)
Studenten/stagaires
Het ELSI onderzoeksteam wordt ondersteund door een wisselende groep van tijdelijke onderzoekers en stagiaires. Het onderzoeksteam is altijd op zoek naar enthousiaste studenten die onderzoek willen doen naar ELSI aspecten van genetica. In de afgelopen jaren hebben studenten met zeer verschillende achtergronden (geneeskunde, psychologie, filosofie, Human Technology, Science Business and Policy, communicatie- en informatiewetenschappen) stage gelopen. Informeer voor mogelijkheden bij Dr. Imke Christiaans (i.christiaans umcg.nl).
Onderzoeksprojecten
ELSI onderzoek wordt gedaan op zeer uiteenlopende onderwerpen. Hieronder wordt informatie gegeven over enkele recente en historische onderzoeksprojecten om dit te verduidelijken.
1. Screening
Recent project: Verantwoorde toepassing van next generation sequencing technieken in screening. Next generation sequencing technieken zoals whole exome sequencing (WES) en whole genome sequencing (WGS) maken het mogelijk om het hele DNA te analyseren. Screening die gebruikt maakt van WES/WGS biedt de mogelijkheid voor uitbreiding van reproductieve keuzes voor en tijdens een zwangerschap, en kan vroege diagnose van behandelbare aandoeningen stimuleren en zo gezondheidswinst opleveren. De toepassing van WES/WGS in screening brengt ook ethische, juridische en maatschappelijke vragen met zich mee. In dit onderzoeksproject zijn via literatuuronderzoek en een empirische en normatieve analyse, uitgevoerd in samenwerking met relevante stakeholders, voorwaarden geïdentificeerd voor verantwoorde toepassing van WES/WGS gebaseerde screening. Verschillende screeningssettings staan hierbij centraal: populatiescreening, opportunistische screening en een commercieel aanbod. Binnen deze screeningssetting wordt onderzocht welke uitbreidingen of aanpassingen nodig zijn van het huidige normatieve screeningskader. Hierbij wordt met name naar vier cruciale aspecten gekeken: informatievoorziening en toestemming, kwaliteit van de screening en nevenbevindingen, hergebruik van gegevens en impact van niet-deelname.
Historisch project: Preconceptie dragerschapsscreening bij gezinsplanning. Een voorbeeld van innovatie in de genetica en de verschillende stappen die in onze onderzoekscyclus worden genomen, is het op grote schaal aanbieden van preconceptie dragerschapsscreening aan mensen met kinderwens. Op 28 juni 2021 promoveerde Juliette Schuurmans op dit onderwerp. Preconceptie dragerschapsscreening biedt paren die een gezin willen stichten de mogelijkheid om voorafgaand aan de zwangerschap na te gaan of zij -als paar- een significant verhoogde kans hebben op kinderen met een ernstige recessief overervende aandoening. Een dergelijke screeningstest was nog niet eerder aangeboden of geëvalueerd in de gezondheidszorg.
Dit werk begon met een internationale multidisciplinaire bijeenkomst van belanghebbenden waarin de deelnemers elkaar op scherp zetten over hoe een verantwoorde test eruit zou moeten zien. Vervolgens heeft het laboratorium een preconceptionele dragerschapstest opgezet. Daarnaast deed de ELSI onderzoeksgroep onderzoek naar de wenselijkheid en voorwaarden voor het aanbieden van zo'n test onder zowel potentiële aanbieders als wensouders. Afgezien van enige aarzeling was er veel enthousiasme. Dit werd opgevolgd door het opzetten, uitvoeren en evalueren van een pilot in Noord-Nederland. De pilot liet zien dat verantwoorde implementatie mogelijk is in een dragerschapstest die door huisartsen wordt aangeboden.
In de volgende stap naar landelijke implementatie heeft ons Nederlandse consortium een Nederlandse richtlijn ontwikkeld en - binnen een ZonMW-studie geïnitieerd door het Ministerie van Volksgezondheid, Welzijn en Sport - een advies gegeven gericht op voorwaarden voor een landelijke proefimplementatie van preconceptie dragerschapsscreening. Dit advies is meegenomen door de Nederlandse Gezondheidsraad in hun rapport over preconceptie dragerschapsscreening van 15 november 2023, waarin wordt voorgesteld om alle paren met een kinderwens deze screening aan te bieden, maar eerst de effectiviteit en haalbaarheid van zo'n landelijk aanbod te evalueren in een pilotstudie.
2. Technologische innovatie
Recent project: Stamboom van je hart. De ELSI onderzoeksgroep ontwikkelt een digitale risicotool die iemands persoonlijke risico op hart- en vaatziekten voorspelt op basis van het voorkomen van hart- en vaatziekten in de familie. De tool richt zich op zowel monogene als complexe multifactoriële hart- en vaatziekten. Door deze tool te implementeren willen we mensen in de algemene bevolking bewust maken van hun persoonlijke risico en mensen met een hoger risico opsporen en doorverwijzen naar hun huisarts voor verdere diagnostiek en behandeling, zodat sterfte door plotselinge hartdood en ernstige ziekteverschijnselen in de toekomst verminderd kunnen worden. De tool zal worden aangevuld met informatie voor huisartsen en zal waarschijnlijk in 2024 worden gelanceerd.
Als eerste stap in de ontwikkeling van de tool brachten experts het wettelijke en ethische kader in kaart en concludeerden dat vooral regelgeving van de Europese Unie (EU) zoals de Verordening Medische Hulpmiddelen en de Algemene Verordening Gegevensbescherming potentiële obstakels vormen voor de ontwikkeling, bredere beschikbaarheid en het algemeen gebruik van de tool. De ethische uitdaging betrof de vraag hoe familieleden van gebruikers te waarschuwen die niet alleen familiegegevens delen met de gebruiker maar mogelijk ook het risico op hart- en vaatziekten. Met behulp van een focusgroep en een Delphi-studie onder klinische experts hebben we familiecriteria ontwikkeld die kunnen wijzen op een verhoogd risico en deze gevalideerd in een cohort met een hoog risico en een algemene populatie cohort. Deze familiecriteria moesten begrijpelijk zijn voor leken en eenvoudig te gebruiken in een digitale tool. Vervolgens zijn twee verschillende prototypes van de tool ontwikkeld en getest op acceptatie en bruikbaarheid in een algemeen bevolkingscohort. Dit project wordt gefinancierd door de Nederlandse Hartstichting.
Recent project: ELSA AI Lab Noord Nederland. Het ELSA AI lab Noord-Nederland (ELSA-NN) richt zich op het onderzoeken van culturele, ethische, juridische, sociaal-politieke en psychologische aspecten van het gebruik van AI in de gezondheidszorg ter bevordering van gezond leven, werken en ouder worden. Door deze aspecten te onderzoeken in verschillende besluitvormingscontexten, de use cases, waaronder één in de genetica, en deze kennis te integreren in een online ELSA-tool, wil ELSA-NN bijdragen aan kennis over betrouwbare mensgerichte AI en de ontwikkeling en implementatie van technologische innovaties in de gezondheidszorg, waaronder AI, in de noordelijke regio.
De genetica use case die binnen het ELSA AI Lab wordt bestudeerd, richt zich op het gebruik van AI bij de interpretatie van DNA-varianten in next generation sequencing gebaseerde screening van pasgeborenen (de hielprikscreening). De huidige screening van pasgeborenen wordt uitgevoerd met behulp van biochemische tests. Met het gebruik van nieuwe DNA-sequencingtechnieken kan bij pasgeborenen worden gescreend op meer ernstige behandelbare ziekten. Sequencing brengt echter ook de interpretatie van veel DNA-varianten per monster met zich mee. Voor een snel testresultaat -binnen een week zoals bij de huidige screening van pasgeborenen- en veel te testen monsters kan AI nuttig zijn bij de interpretatie van DNA-varianten. Welke varianten kunnen ziekte veroorzaken en welke zijn onschuldig? De onderzoekers van het ELSA AI Lab zullen samen met de ELSI-onderzoeksgroep kijken naar juridische aspecten en ethische en psychologische aspecten zoals vertrouwen en acceptatie van AI.
Meer informatie: ELSA AI lab Northern Netherlands (ELSA-NN) (umcgresearch.org)
3. Counseling
Recent project: Informatieverstrekking en vroegtijdige opsporing van familieleden die risico lopen op een erfelijke ziekte. Bij veel erfelijke aandoeningen, vooral autosomaal dominante, is er een risico van 50% voor eerstegraads familieleden van de erfelijke aanleg. Weten dat je de genetische aanleg hebt, kan nuttig zijn voor levensplanning, maar ook voor ziektepreventie. Voor veel erfelijke ziekten, zoals erfelijke kanker en erfelijke hart- en vaatziekten, zijn preventieve maatregelen en/of behandelingen beschikbaar die ernstige symptomen van de ziekte kunnen voorkomen of verminderen. Voor dergelijke behandelbare erfelijke ziekten komt slechts 50% van de familieleden voor DNA-onderzoek naar de erfelijke aanleg. De ELSI-onderzoeksgroep onderzoekt hoe de informatievoorziening aan familieleden kan worden verbeterd, welke andere redenen er kunnen zijn om geen afspraak te maken voor genetische counseling en testen en hoe we familieleden het beste kunnen helpen om een weloverwogen beslissing te nemen over DNA-onderzoek.
Historisch project: Validatie van de Genetic Counseling Outcome Scale. De gezondheidszorg besteedt nu steeds meer aandacht aan het meten van patiëntervaringen, via zogeheten Patient Reported Outcome Measures (PROMs). Er worden reeds verschillende instrumenten ontwikkeld om patiëntervaringen te meten in de gezondheidszorg. Er was echter geen geschikt Nederlands instrument om het effect van genetische counseling op de patiënt te meten. In het Verenigd Koninkrijk was al wel een PROM voor genetische counseling ontwikkeld en gevalideerd -de Genetic Counselling Outcome Scale (GCOS) - die inzicht gaf in de ervaringen van patiënten met genetische counseling. Promovendus Jan Voorwinden heeft een Nederlandse versie van de GCOS gevalideerd onder een grote en diverse groep patiënten. De ELSI onderzoeksgroep heeft plannen om te bestuderen hoe de GCOS gebruikt kan worden om counselingervaringen, patiënt empowerment en gepersonaliseerde zorg verder te verbeteren.
4. Hercontact
Recent project: Farmacogenetisch paspoort. Iemands genetica kan van invloed zijn op hoe goed specifieke medicijnen voor hem of haar werken. Het gebruik van genetische informatie om medicijnen op maat voor te schrijven kan zo helpen bijwerkingen door overdosering of gebrek aan effect door onderdosering te voorkomen. In het farmacogenetisch paspoort project hebben onderzoekers van de afdeling Genetica van het UMCG een route ontwikkeld om deze informatie via een app aan patiënten of het algemene publiek te leveren. De eerste pilot wordt uitgevoerd bij deelnemers van de Lifelines biobank van wie het DNA al beschikbaar is. De ELSI onderzoeksgroep evalueert hoe deelnemers het vinden om informatie te ontvangen over hun genetische medicatiegevoeligheid. Ook willen we weten of de informatie in de app duidelijk en volledig is, zodat we de app in de toekomst nog beter kunnen afstemmen op de behoeften van mensen.
Historisch project: Plicht tot hercontact. Hercontact met patiënten kan gewenst zijn bij nieuwe genetische bevindingen of nieuwe interpretatie van eerdere bevindingen. Er werd een systematische literatuurstudie uitgevoerd naar de plicht tot hercontact en ethische, juridische en psychosociale (ELSI) kwesties hierbij. Dit reviewartikel, gepubliceerd in Genetics in Medicine, toonde aan dat hercontact wenselijk is, maar dat er geen wettelijke plicht is. De praktische aspecten van een hercontactbeleid werden gezien als de belangrijkste belemmering voor de toepassing ervan. In een ander onderzoek hielden we interviews met experts en groepsdiscussies met patiënten en professionals over de plicht tot hercontact en de praktische aspecten. Ook uit dit onderzoek kwam naar voren dat de deelnemers hercontact niet als een plicht zagen, maar dat het wel wenselijk zou kunnen zijn. Daarnaast formuleerden we een aantal eisen waarmee het hercontactbeleid rekening moet houden voor een succesvolle implementatie. Als volgende stap werd een hercontact-app ontwikkeld en geëvalueerd in een kwantitatieve studie onder ongeveer 250 vroegere patiënten. Het doel was om mensen op een efficiënte en verantwoorde manier te hercontacteren wanneer er nieuwe of herziene genetische informatie over hun (potentiële) erfelijke aandoening beschikbaar was. Er zijn essentiële medisch-ethische, psychologische en medisch-juridische vereisten om rekening mee te houden, waaronder hoe vroegere patiënten het hercontact ervaren en welke voorwaarden moeten worden opgenomen in eHealth toepassingen zoals een hercontacting-app.
| Laatst gewijzigd: | 11 maart 2025 14:32 |
