Cholinergic regulation of inflammation and remodelling in asthma and COPD
From molecular mechanism to clinical application
Investigators involved: Reinoud Gosens, Loes Kistemaker, Herman Meurs
Acetylcholine is the primary parasympathetic neurotransmitter in the airways, which induces bronchoconstriction and mucus secretion. The activity of the neuronal system is increased in COPD and asthma. Therefore, anticholinergics are effective bronchodilators in COPD and in asthma.
Recent data are changing this traditional view: resident and inflammatory cells that control inflammation and remodelling produce acetylcholine and express muscarinic receptors. Moreover, anticholinergics reduce neutrophilia and small airway remodelling in animal models of COPD, and eosinophilia and airway remodelling in animal models of allergic asthma. Although the clinical significance of these findings is not yet fully determined, a pro-inflammatory role for acetylcholine could explain the aforementioned effects of anticholinergics on exacerbations and fits with our recent clinical data suggesting anti-inflammatory effects of targeted lung denervation in patients with COPD. Whether anticholinergics can be anti-inflammatory in patients with COPD as well is currently under investigation.
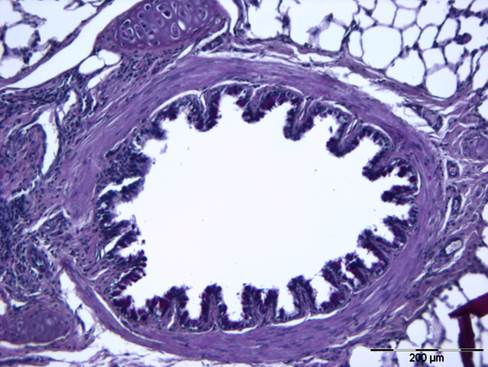
The mechanisms involved are not completely understood yet; however, we recently demonstrated that the muscarinic M3 receptor plays a dominant role in the inflammatory response induced by cigarette smoke in mice and studies with bone-marrow chimeric mice clearly indicate a role for the M3 receptor on structural cells in this response. The same holds true for the role of muscarinic receptors in allergen-induced inflammation and remodelling, where anticholinergics or M3 knock-out have particularly profound effects on airway smooth muscle thickening, on mucus hypersecretion and on eosinophilic inflammation. These effects may in part be regulated by mechanical effects resultant from bronchoconstriction. This suggests that patients with COPD or asthma might benefit from anticholinergic therapy to a much larger extent than previously appreciated. We are presently investigating these molecular mechanisms and the clinical implications and applications.
Relevant literature:
Acetylcholine beyond bronchoconstriction: roles in inflammation and remodeling. Kistemaker LE, Gosens R. Trends Pharmacol Sci. 2015 36(3):164-171.
Bronchoconstriction and airway biology: potential impact and therapeutic opportunities. Gosens R, Grainge C. Chest. 2015 147:798-803.
Anti-inflammatory effects of targeted lung denervation in patients with COPD. Kistemaker LE, Slebos DJ, Meurs H, Kerstjens HA, Gosens R. Eur Respir J. 2015 46:1489-1492.
| Last modified: | 06 October 2017 10.54 a.m. |
