
Introduction & Mission
Classically immunology and endocrinology have been separate entities in biomedical and clinical research. During the past decade however it has become more and more clear that many processes in the endocrine and in the immune system are steered by hormones as well as by cytokines. For example the quality of the immune system in the intestine depends not only on cytokines but also on locally produced hormones and molecules produced by the microbes in the intestines. The fact that 75% of the lymphocytes in the human body are located and mature in the gut illustrates the importance of the immunoendocrinology of the gut for human health.
The mission of the immunoendocrinology group is to understand the complex interaction between the immune and the endocrine systems in specific targeted areas. These areas are outlined below and are being steered by dedicated principal investigators.
Nutritional immunology; how can specific food components influence the immune barrier of the gastrointestinal tract.
Approximately 80% of all infections enter the human body via the gastrointestinal tract. The cells in the mucosal immune system are usually in high alert status to delete the intruders. This however holds the threat of undesired inflammatory responses. To prevent this the mucosal immune system is controlled by many cytokines and hormones to keep a tight balance between effector and regulatory responses. The quality and alertness of the components are dependent on the intake of food. Especially fibers and molecules on microbes are of crucial importance for keeping the balances in the mucosal immune system under tight control. We have a technology platform in which we study the effect of food components on (i) mucus production and function, (ii) epithelial integrity, (iii) stimulation of specific repertoires of pattern recognition receptors, and (iv) innate and adaptive responses in mice and humans.
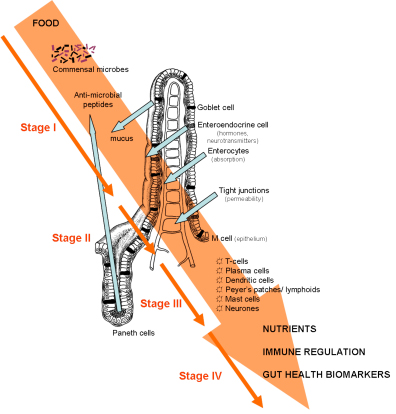
The different barriers in the gastrointestinal tract that both pathogens and food components have to pass in order to influence the human immune and endocrine system.
Pregnancy immunology; how does pregnancy influence the immune response and how does the immune response influence pregnancy
The acceptance of the semi allogeneic fetus depends on the adaptations in the maternal immune response to pregnancy. Adaptations in the maternal immune response involve a shift from the cellular immune response towards a humoral immune response, an increase in regulatory T cells and a generalized activated innate immune response. Maladaptation of the maternal immune response to pregnancy usually results in pregnancy-complications, such as preeclampsia or fetal growth restriction. In the immunoendocrinology section we study how the maternal immune response adapts to pregnancy and which pregnancy factors induce these adaptations in both human and animal models. Many factors may be involved, such as hormones and other factors produced by the placenta or the ovaries. Moreover, we also study how maladaptations of the immune response or activation of the immune response influences pregnancies and induce pregnancy complications such as preeclampsia.
Since reproductive hormones, such as oestrogen and progesterone have been shown to be important in the regulation of the immune response during pregnancy, it is also important to study the effect of these hormones on the immune response in various reproductive condition, apart from pregnancy. Therefore we also focus on the effect of the reproductive condition on immune response, we for instance study gender differences in immune responses, but also differences in immune responses within the female menstrual cycle.
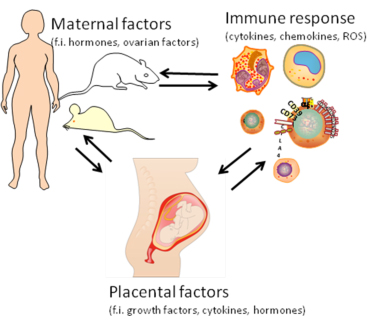
Placental factors, factors produced by activated immune cells and maternal factors do all affect each other and are together responsible for the acceptance of the semiallogeneic fetus and a healthy pregnancy
Immunology of cell transplants; what causes the strong rejection of cellular grafts of islets of Langerhans and can this prevented with encapsulation.
Our laboratory has a 20 years history in experimental islet-cell transplantation research. A strong focus is the development of immuno isolating capsules for preventing rejection of pancreatic islets. We are connected to the immunoendocrinology section as factors responsible for rejection of immuno isolated islets are not only related to foreign body responses but mainly due to hormones and cytokines produced by the islets themselves. We are able to produce capsules that stay free of any any cell adhesion for the life span of experimental animals such as mice, rats, and pigs. However when islets are placed in the capsules we found that up to 60% of the islets may be lost in the first two weeks after transplantation due to stress hormones and cytokines produced by the islets. We study the etiology and pathogenesis of failure of (non)encapsulated islet grafts in detail since we belief that understanding the factors contributing to success and failure is the shortest way to develop strategies to prevent failure. At present we have projects that focus on prevention of loss of islets in the immediate post transplant period. Novel immuno isolation processes and temporary release of beneficial factors to promote islet survival have been developed for this purpose.
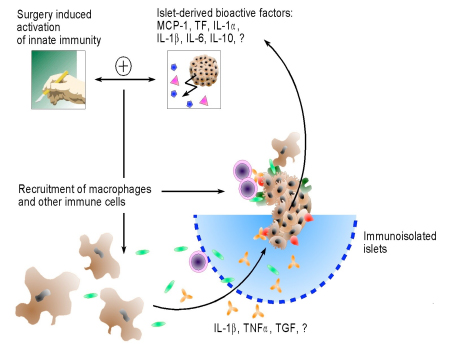
The complex immunoendocrinology of the etiology of loss of islets in the presence or absence of immuno isolating capsules.
More information on our scientists and laboratory technicians, and an overview of relevant publications can be found in the menu at the left.
| Last modified: | 05 November 2013 1.28 p.m. |
