How carbohydrates make infant formula more like human breast milk
University of Groningen scientists have discovered how a class of carbohydrates (galactooligosaccharides) helps infant formula to stimulate the gut microbiota of babies in a similar way that breast milk does. These carbohydrates kick-start the pathways that bacteria use to digest mucus, thereby increasing the chance of survival of these bacteria in the gut. This finding, which the University has patented, paves the way for using these ‘prebiotics’ to increase the nutritional value of infant food. The results were published in the journal Scientific Reports on 16 January.

Infant formula, which is usually based on cow’s milk, does not stimulate the gut microbiota in the same way breast milk does. Adding a mixture of human milk oligosaccharides (HMOs) helps, but these carbohydrates are expensive and challenging to make. Infant formula producers have discovered that cheaper carbohydrates (galactooligosaccharides, GOS) have a similar effect, despite being very dissimilar in structure to the HMOs.
Energy
‘No one knew why these carbohydrate mixtures elicited the same response. So we decided to investigate’, says Alicia Lammerts van Bueren, first author of the study and the recipient of an NWO Veni grant. She used a gut bacterium, Bacteroides thetaiotaomicron, as a model system. This microorganism has some 400 genes for carbohydrate digestion, whereas humans have only ten. In the human gut, such bacteria break down indigestible carbohydrates allowing us to use them for energy production.
‘The genome of B. thetaiotaomicron is well known and encodes a large number of pathways specialized in the degradation of particular carbohydrates’, explains Lammerts van Bueren. ‘By looking at the expression of these different pathways, we can use them as indicators of the type of response that different carbohydrates cause.’
The bacteria were exposed to either HMOs or GOS. By looking at the proteins the cells produced in response, it was possible to deduce which pathways became active. Both stimulated the expression of a pathway used to digest mucin glycoproteins (mucin degradative pathways) whereas GOS also stimulated the expression of another pathway used to break down pectin (polysaccharide with galactose units).
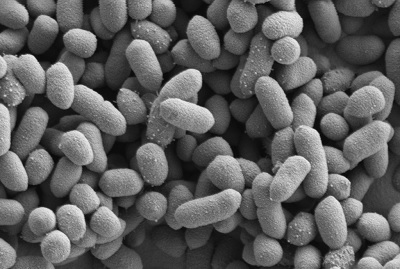
‘So it appears that the activation of the mucin pathways is vital to the positive effect on the gut microbiota’, says Lammerts van Bueren. ‘We suggest that both HMOs and GOS activate the mucin pathway, which gives the bacteria an advantage as they are then able to live off the abundant mucin in the gut.’ Mucus is slow to activate the mucin pathway, whereas the prebiotics are much faster. ‘This kick-starts the ability of the bacteria to feed off mucin.’
Oddly enough, HMOs and GOS have different structures, and both also differ from mucin. ‘They appear to share structural attributes which make them bind to some sort of inducer for mucin degradation in these bacteria. But you couldn’t have predicted this from the structural formulas of these oligosaccharides.’
The scientists have managed to identify the specific GOS compounds that activate the mucin pathway and have applied for a patent for this compound and its use. Several producers of infant formula have expressed interest in the work of Lammerts van Bueren and her colleagues in the Microbiology research group at the University of Groningen.
Reference: Alicia Lammerts van Bueren, Marieke Mulder, Sander van Leeuwen & Lubbert Dijkhuizen: Prebiotic galactooligosaccharides activate mucin and pectic galactan utilization pathways in the human gut symbiont Bacteroides thetaiotaomicron. Scientific Reports, 16 January 2017, DOI 10.1038/srep40478
| Last modified: | 11 February 2025 2.52 p.m. |
More news
-
29 August 2025
Top Dutch Solar Racing stranded just before the finish line, but returns proudly
From August 24 to 31 this year, the student team Top Dutch Solar Racing will participate in the Bridgestone World Solar Challenge. This page will keep you up to date on the latest developments during and around the race.
-
21 August 2025
Upconversion nanoparticles to aid the application of molecular motors
Scientists from Groningen University and the University of Amsterdam have developed upconversion nanoparticles to assist in powering molecular motors.
-
19 August 2025
Bruno Ehrler appointed new director of AMOLF
Honorary professor Bruno Ehrler of the University of Groningen has been appointed as the new director of AMOLF, the NWO Institute for research into functional complex matter.
